Search


Ending the HIV Epidemic
Ending the HIV Epidemic in the U.S. (EHE) is a bold plan announced in 2019 that aims to end the HIV epidemic in the United States by 2030. Agencies across the U.S. Department of Health and Human Services (HHS) developed an operational plan to pursue that goal accompanied by a request for additional funding.
The plan leverages critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response by coordinating the highly successful programs, resources, and infrastructure of many HHA agencies and offices. Initially, the initiative is focusing on areas where HIV transmission occurs most frequently, providing 57 geographic focus areas with an infusion of additional resources, expertise, and technology to develop and implement locally tailored EHE plans.
Goal
The initiative seeks to reduce the number of new HIV infections in the United States by 75 percent by 2025, and then by at least 90 percent by 2030, for an estimated 250,000 total HIV infections averted.

HIV in America
HIV has cost America too much for too long and remains a significant public health issue.
- More than 700,000 American lives have been lost to HIV since 1981.
- More than 1.1 million Americans are currently living with HIV and many more are at risk of HIV infection.
- While new HIV diagnoses have declined significantly from their peak, progress on further reducing them has stalled with an estimated 38,000 Americans being newly diagnosed each year. Without intervention nearly 400,000 more Americans will be newly diagnosed over 10 years despite the availability of tools to prevent transmissions.
- The U.S. government spends $20 billion in annual direct health expenditures for HIV prevention and care.
- There is a real risk of an HIV resurgence due to several factors, including trends in injection and other drug use; HIV-related stigma; homophobia and transphobia; lack of access to HIV prevention, testing, and treatment; and a lack of awareness that HIV remains a significant public health threat.
Learn more about the latest statistics on new HIV diagnoses, people with HIV, and AIDS diagnoses and deaths in the United States and learn about the impact of HIV on racial and ethnic minorities.
Right Data & Right Tools
Data tells us that most new HIV infections occur in a limited number of counties and among specific populations, giving us the information needed to target our efforts to those locales that will make the biggest impact on ending the HIV epidemic. Further, today we have the tools available to end the HIV epidemic. Landmark biomedical and scientific research advances have led to the development of many successful HIV treatment regimens, prevention strategies, and improved care for persons with HIV. Notably:
Thanks to advances in antiretroviral therapy, the medicine used to treat HIV, people with HIV who take HIV medicine as prescribed and, as a result, maintain get and keep an undetectable viral load can live long and healthy lives and will not transmit HIV to an HIV-negative partner through sex.
We have proven models of effective HIV care and prevention based on more than two decades of experience engaging and retaining patients in effective care.
Pre-exposure prophylaxis (PrEP), a daily regimen of two oral antiretroviral drugs in a single pill, has proven to be highly effective in preventing HIV infection for individuals at high risk, reducing the risk of acquiring HIV by up to 97 percent. A long-acting injectable form of PrEP has also been approved by the FDA.
Syringe services programs (SSPs) dramatically reduce HIV risk and can provide an entry point for a range of services to help stop drug use, overdose deaths, and infectious diseases.
New laboratory and epidemiological techniques allow us to pinpoint where HIV infections are spreading most rapidly so health officials can respond swiftly with resources to stop the further spread of new transmissions and support those newly diagnosed.
With these powerful data and tools, we have a once-in-a-generation opportunity to end the HIV epidemic.
HHS Leadership
This initiative is leveraging critical scientific advances in HIV prevention, diagnosis, treatment, and care by coordinating the highly successful programs, resources, and infrastructure of many HHS agencies and offices, including the:
The HHS Office of the Assistant Secretary for Health is coordinating this cross-agency initiative.
Whole-of-Society Initiative
Achieving EHE’s goals will require a whole-of-society effort. In addition to the coordination across HHS agencies, the success of this initiative will also depend on dedicated partners from all sectors of society working together, including people with HIV or at risk for HIV; city, county, tribal, and state health departments and other agencies; local clinics and healthcare facilities; healthcare providers; providers of medication-assisted treatment for opioid use disorder; professional associations; advocates; community- and faith-based organizations; and academic and research institutions, among others. Engagement of community in developing and implementing jurisdictional EHE plans as well as in the planning, design, and delivery of local HIV prevention and care services is vital to the initiative’s success.
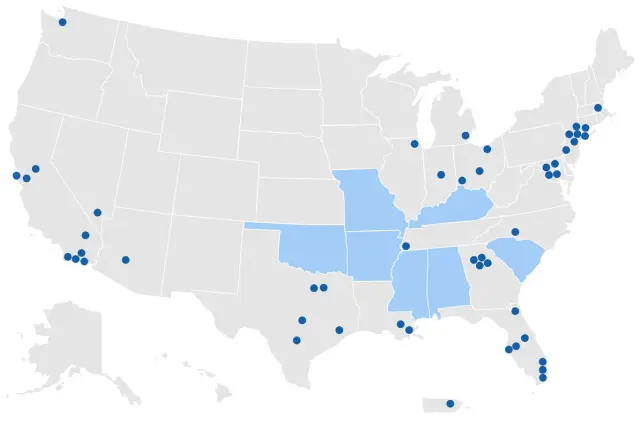
Read a list of the 48 counties with the highest number of new HIV diagnoses, as well as Washington, DC, and San Juan, Puerto Rico and the seven states with a high proportion of HIV diagnoses in rural areas.
EHE States, Counties, and Territories (PDF 44 KB)
Priority Jurisdictions
Initially, the EHE initiative will focus on 57 priority jurisdictions, including 48 counties, Washington, DC, and San Juan, Puerto Rico, where more than 50 percent of new HIV diagnoses occurred in 2016 and 2017, and also seven states with a disproportionate occurrence of HIV in rural areas. Subsequently, efforts will expand more widely across the nation to reduce new infections by 90 percent by 2030. Ultimately, intensive case management will be implemented to maintain the number of new infections at fewer than 3,000 per year.
Learn more about EHE Priority Jurisdictions.Key Strategies
The Ending the HIV Epidemic initiative focuses on four key strategies that, implemented together, can end the HIV epidemic in the U.S.: Diagnose, Treat, Prevent, and Respond.
Read about the Key EHE Strategies.Funding
Congress approved some additional HIV resources in fiscal years 2020, 2021, and 2022 to support this multiyear initiative focused on ending the HIV epidemic in America by 2030.
Read more about the funding for the EHE initiative.Challenges
Despite the game-changing developments in HIV prevention and treatment tools, not everyone is benefiting equally from these advances. New infections are highly concentrated among men who have sex with men; minorities, especially African Americans, Hispanics/Latinos, and American Indians and Alaska Natives; and those who live in the southern United States.
Further, analysis from CDC shows the vast majority (about 80 percent) of new HIV infections in the U.S. in 2016 were transmitted from the nearly 40 percent of people with HIV who either did not know they had HIV, or who had been diagnosed but were not receiving HIV care. These data underscore the impact of undiagnosed and untreated HIV in the nation and also the critical need to expand HIV testing and treatment in the United States.
Fact Sheet
And stigma—which can be a debilitating barrier preventing people with or at risk for HIV from receiving the health care, services, and respect they need and deserve—still tragically surrounds HIV. Responding to HIV is not just a biomedical issue, but a social challenge, too.
Effective interventions have driven the number of new HIV infections down to approximately 35,000 per year—the lowest level ever. However, recent data show that our our progress reducing the number of new HIV infections has plateaued. Now there are new threats to the progress we’ve made, the most significant being the opioid crisis: One in 10 new HIV infections occurs among people who inject drugs.
Our Opportunity
Our nation faces an unprecedented opportunity once thought impossible. The most powerful HIV prevention and treatment tools in history are now available. Areas where HIV transmission is occurring most rapidly can also be identified.
By deploying those tools swiftly and to greatest effect, the HIV epidemic in America can end.









